 When someone we care about is going through a difficult time, it can be challenging to know what to say or how to help. We may worry about saying the wrong thing, making things worse, or appearing insensitive. It’s natural to feel this way because we want to offer support and comfort, but we also don’t want to make things worse.
When someone we care about is going through a difficult time, it can be challenging to know what to say or how to help. We may worry about saying the wrong thing, making things worse, or appearing insensitive. It’s natural to feel this way because we want to offer support and comfort, but we also don’t want to make things worse.
The truth is that there is no magic phrase or solution that will fix everything. However, acknowledging their pain and letting them know that you are there for them can be a powerful show of support. Sometimes, simply listening without judgment can help someone feel heard and validated.
Ultimately, the most important thing is to be genuine and empathetic. You don’t have to have all the answers, but showing that you care and are willing to be there can make a world of difference to someone who is struggling.
Category: Uncategorized
 What is substance addiction?
What is substance addiction?
At its core, it involves a compulsive need for drugs or alcohol, often leading to continued use despite adverse consequences. It is usually associated with a psychological as well as physical dependence.![]() Identifying the signs of substance addiction is a crucial step toward intervention and recovery. Keep an eye out for these indicators:
Identifying the signs of substance addiction is a crucial step toward intervention and recovery. Keep an eye out for these indicators:
Behavioral Changes: Sudden shifts in behavior, priorities, and interests.
Neglect of Responsibilities: A decline in fulfilling personal, professional, or social obligations.
Secrecy and Isolation: Attempts to conceal substance use and withdrawing from social connections.
Increased Tolerance: Needing more of the substance to achieve the same effect.
Withdrawal Symptoms: Physical and psychological distress when not using the substance.
Persistent Cravings: Overwhelming urges to engage in substance use.![]() Starting the Conversation:
Starting the Conversation:
Breaking the silence surrounding substance addiction is important. Engaging in open, non-judgmental conversations fosters an environment where individuals feel comfortable seeking help. It’s not just about identifying the issue; it’s about creating a space for understanding and support.![]() Compassionate Support is Key:
Compassionate Support is Key:
If you or someone you know resonates with these signs, remember that help is available. Seeking professional support, whether through a primary care provider, therapy, or support groups, is a courageous step toward a healthier future.
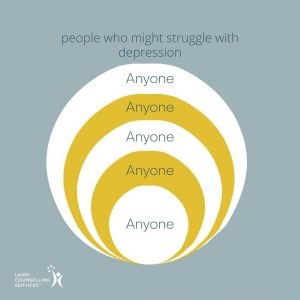 Depression is a mood disorder that can affect anyone, regardless of age, gender, ethnicity, or socioeconomic background. It is not a sign of weakness or failure, but rather a complex condition caused by a combination of genetic, environmental, and psychological factors.
Depression is a mood disorder that can affect anyone, regardless of age, gender, ethnicity, or socioeconomic background. It is not a sign of weakness or failure, but rather a complex condition caused by a combination of genetic, environmental, and psychological factors.
People who struggle with depression may experience a range of symptoms, such as a persistent feeling of sadness or emptiness, loss of interest in activities they once enjoyed, changes in appetite and sleep patterns, low energy and fatigue, difficulty concentrating, feelings of worthlessness or guilt, and even thoughts of suicide.
Depression can be triggered by various life events, such as the loss of a loved one, a major life transition, or chronic stress. It can also be associated with underlying medical conditions, such as thyroid disorders, chronic pain, or substance abuse.
Treatment for depression may involve a combination of therapy, medication, and lifestyle changes. It is important to seek help if you or someone you know is struggling with depression, as it is a treatable condition that can improve with proper care and support.
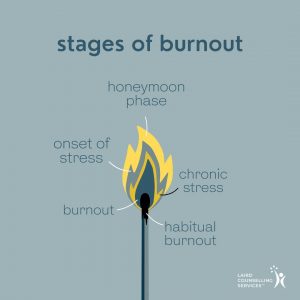 Burnout is a state of physical, mental, and emotional exhaustion caused by prolonged stress. It is characterized by feelings of cynicism, detachment, and ineffectiveness.
Burnout is a state of physical, mental, and emotional exhaustion caused by prolonged stress. It is characterized by feelings of cynicism, detachment, and ineffectiveness.
Burnout typically occurs in stages. The first stage is the “honeymoon” phase, characterized by enthusiasm and high energy. The second stage is the “onset of stress” phase, where stress levels begin to increase, and individuals may experience irritability, anxiety, and lack of focus. The third stage is the “chronic stress” phase, where burnout symptoms become more severe, such as chronic fatigue, insomnia, and physical illness. From there, you get into full-fledged burnout, which can become habitual.
If you’re experiencing burnout, it’s important to take action. Start by acknowledging your feelings and identifying the source of stress. Practice self-care by getting enough sleep, exercising, and eating well. Set boundaries and prioritize your time. Seek support from loved ones, a therapist, or a support group. Consider taking a break or changing your work environment. Remember, burnout is treatable, and with the right support, it’s possible to recover and avoid future burnout.
Binge eating disorder (BED) is a serious mental health condition that is frequently overlooked and poorly understood. It is a chronic pattern of eating objectively large amounts of food at one time, often in a rushed and secretive way followed by a deep sense of shame. It is estimated to affect about 70 million people worldwide (Keski-Rahkonen, 2021). Although it is not a new phenomenon, there’s a lack of awareness and discussion about BED, leading to stigmatization and barriers to seeking help.
To be clear, two cookies is not a binge. Sometimes guilt can arise from eating a small amount of food, especially if you consider it to be a “bad” food. Volume is the key to distinguishing between a subjective binge and objective binge. As a general guideline, an objective binge is an amount of food that the general population would agree is a lot to consume in one sitting. Binge eating is different from occasional overeating such as feasting during the holidays or celebrating important events. To qualify as BED, binging must occur at least once a week over a period of at least three months and includes a feeling of being out of control.
BED can make you feel very alone because you think you are the only one in the world to have this out-of-control problem with food. A standard reaction would be to hide what and how much you eat out of shame and embarrassment. BED often leads to eating only small portions of food around others, skipping meals or going for long periods of time without eating to then binge when you are alone. During a binge, which can happen once a week or more than once a day, you will eat quickly until uncomfortably full. Binging can be triggered by either negative or positive emotions and is frequently followed by emotional numbness.
Research shows there is a genetic component to eating disorders including BED. If a family member struggled with food or body image, or other mental health issues like anxiety or depression, there is a greater likelihood of developing an eating disorder. Environmental factors such as social media, fashion, beauty, and the health and fitness industry place great emphasis on body image, which increases vulnerability to BED. Psychological factors such as perfectionism (pressure to achieve) and social comparison (comparing what you eat and how you look to others) also play a big role, as does the pressure to conform to cis-gendered body types.
BED alienates you from vital sources of support like loved ones or healthcare professionals because it can be distressing to share the details of your relationship with food. Depression and misuse of substance or alcohol are often found concurrently with BED. Onset of BED can begin in adolescence or adulthood. While some people can talk about it, most go for years without telling anyone in the hope that they will be able to solve the problem on their own by increasing their willpower. Typical self-help strategies to get over binging include different forms of food restriction which only exacerbates the problem. Finding someone you trust is a key place to start. Talk to your doctor and seek out other mental health professionals like a counsellor, registered dietitian, or eating disorder support groups like Body Brave or CMHA-WW.
If you are looking for treatment for BED, there are a variety of therapeutic interventions shown to be effective like cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and interpersonal therapy (IPT) (Iacovino,et al. 2012). CBT addresses negative thought patterns and feelings that result in coping with binging eating. DBT promotes emotional self-regulation, stronger interpersonal skills, mindful self-awareness, and stress management to reduce likelihood of binging. Interpersonal therapy improves interpersonal functioning by addressing relational challenges.
While BED is marked by feelings of helplessness and frustration, there are things you can do that help. Engaging in daily self-care is a primary strategy that reduces vulnerability to binging. Self-care is different for everyone, but it starts with the basics like taking care of your physical needs by showering, eating regularly and getting enough sleep. Self-care also involves building interpersonal skills like setting boundaries and being more assertive. When you feel the urge to binge, try different coping skills such as self-soothing with smelling essential oils, applying a scented lotion, or lighting a scented candle. Resting, stretching, reading, calling a friend, or doing a hobby are other ways of quelling the urge to eat. Of all these tools, doing a hobby can feel the most difficult because hobbies and interests are often the first thing to go with eating disorders. To get back into your hobbies, spend some time remembering what you once loved to do in your free time. If you can’t recall, develop new leisure time activities altogether. If you have been putting your life on hold because of your body image concerns or your relationship with food, start with small steps to built confidence. Some realistic goals for yourself might be going to a movie with a friend or joining a book club. Ultimately, becoming involved in your interests will give you more ways to deal with the feelings that trigger binge eating.
Binge eating disorder can be overcome, and breaking the silence is an important factor in helping yourself and others. By fostering open conversations, reducing stigma, and encouraging those affected to seek help, we can create a supportive environment for healing and recovery.
Remember, seeking help is a courageous step towards regaining control and improving mental and physical well-being. Remember BED flourishes in silence. The first step is to reach out to someone you trust. Connect with your primary care provider or an eating disorder specialist for guidance and support.
References
Keski-Rahkonen, A., (2021), Epidemiology of binge eating disorder: prevalence, course,
comorbidity, and risk factors, Current Opinions in Psychiatry, 34(6), 525-531. Retrieved on
December 10, 2023 from https://pubmed.ncbi.nlm.nih.gov/34494972/
Iacovino, J, M., Gredysa, D. M., Altman, M., & Wilfley, D. E. (2012). Psychological treatments for
binge eating disorder. Current Psychiatry Reports, 14(4), 432–446. Retrieved on December 12, 2023 from doi: 10.1007/s11920-012-0277-8
Iqbal, A. & Rehman, A., (2022), National Library of Medicine: National Center for Biotechnology Information. Binge Eating Disorder. Retrieved on 2023, December 17 from
https://www.ncbi.nlm.nih.gov/books/NBK551700/
National Eating Disorders Information Centre. Affirming Care for Every Body. Retrieved on 2023, December 10 from https://nedic.ca/2slgbtq/
I hope you enjoy this podcast hosted by my good friend and colleague Sarah J. Covey of Covey Wellness Centre. It features another good friend and colleague, Julia Woito, who is a fitness instructor and psychotherapist. Together we explore the difference between exercise and movement and encourage our listeners to find ways to move that is in tune with their bodies and supports positive mental and physical health goals.
Stress is a normal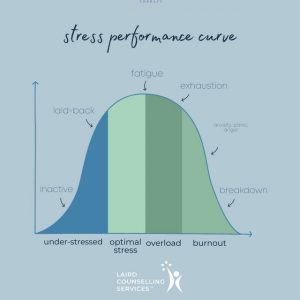 part of life. We all experience it. Stress can be good—it helps us prepare for things that are important to us, like taking a test or going on a job interview.
part of life. We all experience it. Stress can be good—it helps us prepare for things that are important to us, like taking a test or going on a job interview.
But sometimes, stress can feel overwhelming and make you feel like you’re not in control of your emotions or your body. When this happens, it can affect your mental health—and the way you think about yourself and the world around you. The good news is that there are things you can do when stress gets overwhelming so that it doesn’t take over your life.
If you’re feeling overwhelmed or stressed, try these tips:
-Take a quick break and walk away from your situation. This can help you clear your mind and calm down.
-Pause to breathe deeply, focusing on inhaling and exhaling slowly. This will help lower your heart rate and blood pressure, which will make you feel more relaxed.
-Talk with someone about how you’re feeling—it might be a friend or family member who is supportive of you.
-Do something fun to take your mind off things—go for a walk, do a puzzle, or play with your pet.
-Get some exercise; it will help clear your head and shift stress out of your body.
Usually, when you try simple stress-reduction techniques like these, it can help you feel more relaxed, and then you can use that feeling to help you think about your situation differently.
If you find yourself dealing with chronic stress, it might be time to connect with a mental health professional who can help you find ways to manage your stress more effectively.
We are constantly b ombarded with unrealistic and unhealthy standards for what our bodies “should” look like. When we internalize these unrealistic and unhealthy standards, it makes it incredibly difficult to ever achieve confidence in our own bodies.
ombarded with unrealistic and unhealthy standards for what our bodies “should” look like. When we internalize these unrealistic and unhealthy standards, it makes it incredibly difficult to ever achieve confidence in our own bodies.
This can lead to feelings of failure, creating a spiral that damages self-esteem and self-confidence and affects other areas of life like relationships, performance and health.
Restoring your relationship with your body is part of a larger journey to reclaim your right to enjoy life unrestricted by internalized messages of how you “should” look.
You may have been taught “the rules” about what’s acceptable or unacceptable about your body from a young age by society or through the media. You may also have been told throughout your life that certain parts of yourself are not acceptable or attractive because they don’t fit into someone else’s idea of what a body “should” look like.
And at the same time, you may also feel ashamed or embarrassed by these thoughts and beliefs. But it is important not to be hard on yourself because it takes time to change old habits and beliefs about our bodies.
Many people have spent years thinking these things about themselves without even realizing how much damage this has caused them over time until they begin to pay attention.
The first step is realizing that these thoughts are not true, and the second is to replace them with new beliefs about yourself that are more positive and empowering.
Anx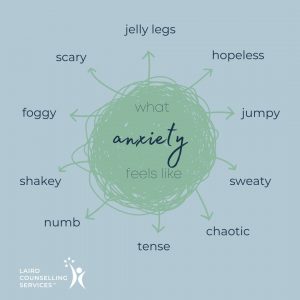 iety is a normal feeling.
iety is a normal feeling.
But sometimes it can get away on us, and start to get in the way of life.
Noticing the way anxiety feels in your body can help you identify when you’re beginning to feel anxious. And if you can tune into those feelings, you can begin to address them before they take over completely.
Anxiety might feel like: jumpiness, sweating, restlessness, tension, numbness, fogginess. It might feel like clenched muscles, shallow breathing, or a stomach ache. Or something else completely!
How does anxiety feel in your body? What grounding techniques do you use when it shows up?
